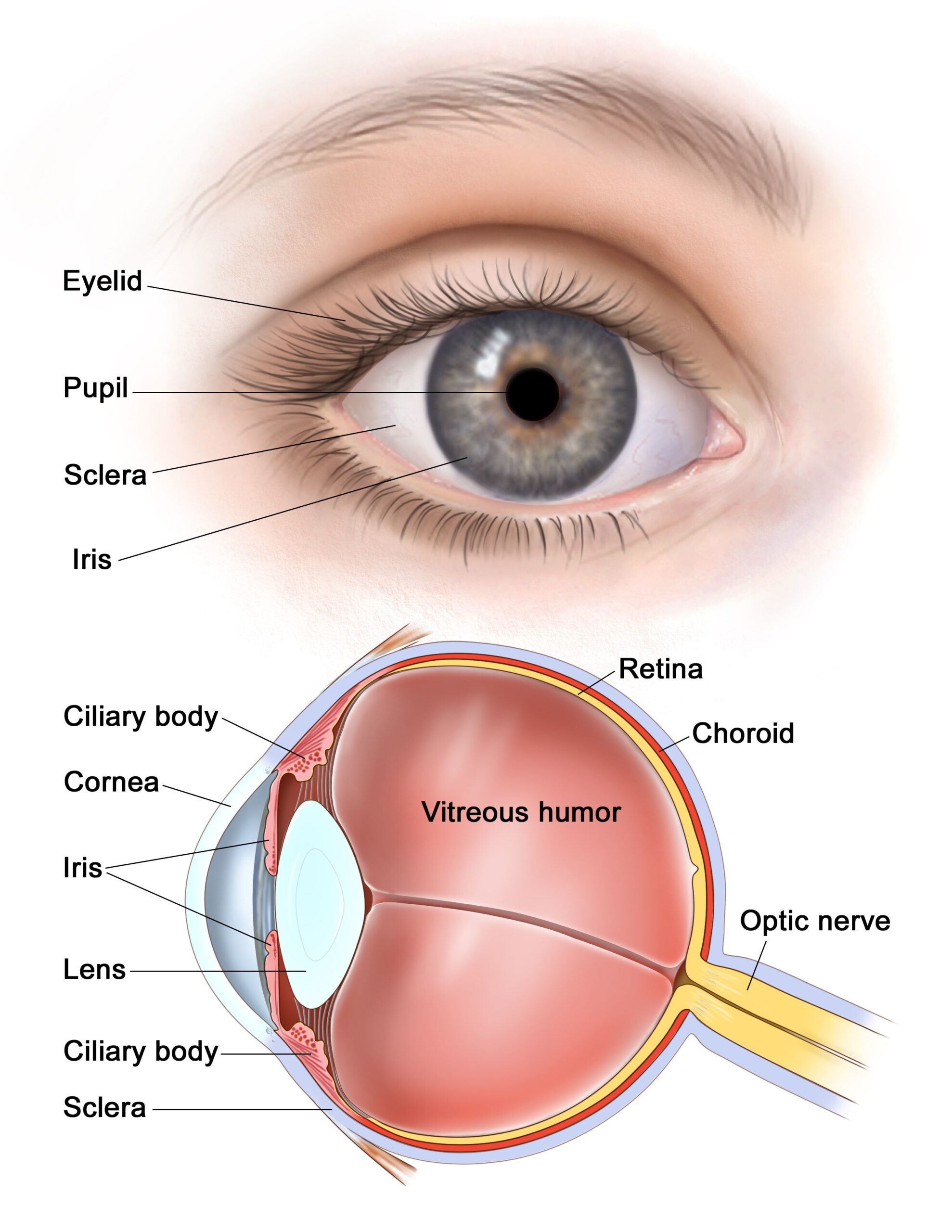
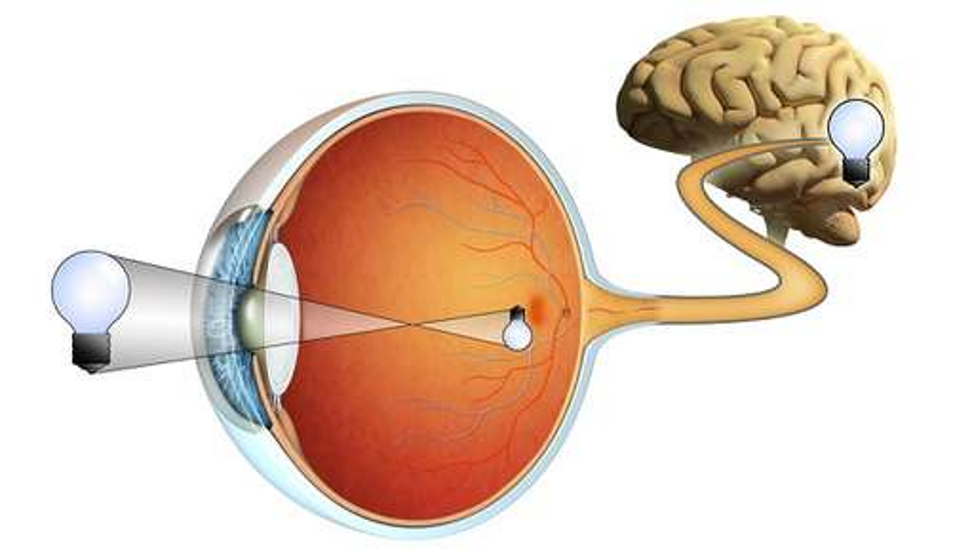
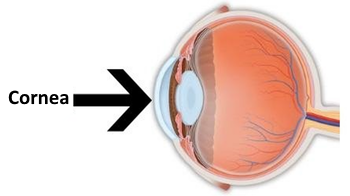
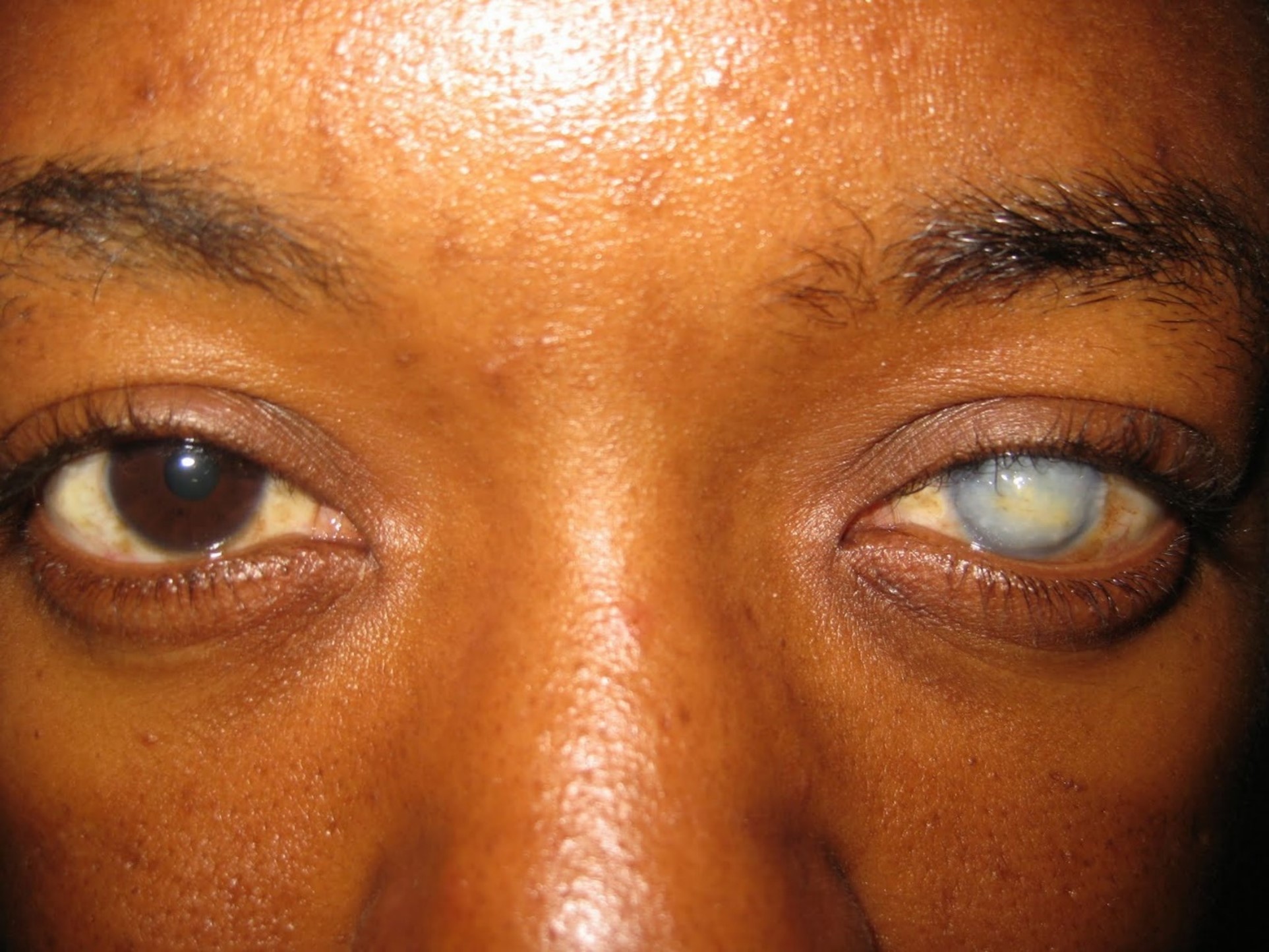
Corneal opacity is a disorder of the cornea. The cornea is the transparent structure on the front of the eyeball. Corneal opacity occurs when the cornea becomes scarred. This stops light from passing through the cornea to the retina and may cause the cornea to appear white or clouded over.
Causes:
- Congenital opacities may occur as developmental anomalies or following birth trauma.
- Ocular trauma
- Corneal Ulceration
- Xerophthalmia
- Infections (i.e Trachoma, Onchocerciasis)
- Mucous membrane pemphigoid
Cases:



Risks:
- Vitamin A Deficiency
- Measels
- Herpes Simplex Virus
- Other infections effecting eyes
- Ocular Trauma and Injuries
- Prolonged use of Contact Lenses
- Keratoconus
- Stevens-Johnson syndrome
- Birth Defects
Kertaoplasty
Keratoplasty also known as corneal transplantation is the main treatment option for visual improvement in corneal opacity. In this, the opaque cornea is replaced with donor tissue. Depending on type and density of corneal opacity different types of keratoplasty may be used.
Keratoprosthetics
Keratoprosthesis is a surgical procedure where a diseased cornea is replaced with an artificial cornea. Traditionally, keratoprosthesis is recommended after a person has had a failure of one or more donor corneal transplants.
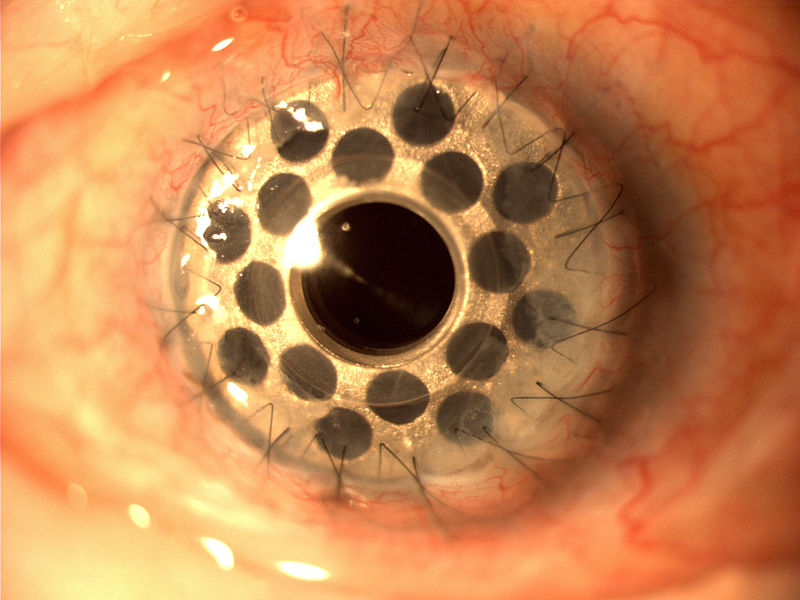
Image above shows a artificial cornea (Boston KPro) made of acrylic plastic.
Keratoprosthesis is reserved for individuals who are not candidates for traditional corneal transplant procedures.

